RESULTS
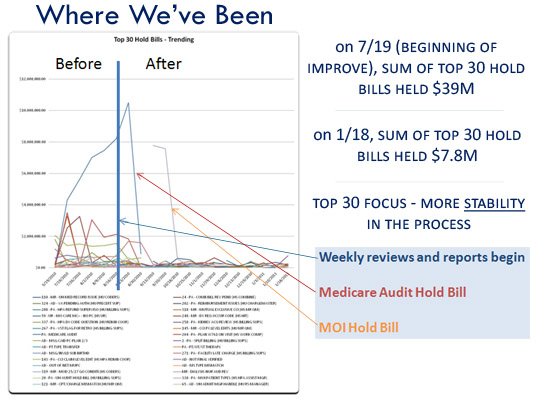
While all phases of the project are not yet completed, the team has already exceeded the goal set for the end of this year and is more than half way to its incremental goal for the end of the fiscal year. Unbilled Days have been reduced from the baseline of 23 to 13.3 at the start of November.
According to the team, “we instituted a few things that we are doing on an ongoing basis:
1. The review meetings are shifting focus from highest dollars in bill holds to those outside of an expected range for that bill hold. While we will still look at high dollar edits, we will focus more on those that have spiked above where we expect them using a ‘control chart’ for each of the edits that have been stabilized.
2. We do weekly “deep dives” where we audit visits and look for process issues. These deep dives initially focused on visits with unbilled balances greater than 30 days from discharge (driven by process issues like late charges, denials or rebills to payers primarily) and are now focused on those where claims are not produced within the expected timeframe of within 8 days from discharge.
3. We continue to brainstorm and seek input from the team and departments in the revenue cycle and look at processes where we can streamline, automate or eliminate edits (without increasing denials, of course).

